About Glaucoma Eye Surgery
What are the types of Glaucoma?
This means their risk of getting glaucoma is higher than normal. Regular eye exams are important to find early signs of damage to their optic nerve. Symptoms-
No symptoms in early stages
Gradually, patchy blind spots in your side vision. Side vision also is known as peripheral vision
In later stages, difficulty seeing things in your central vision
Severe headache
Severe eye pain
Nausea or vomiting
Blurred vision
Halos or colored rings around lights
Eye redness
What causes glaucoma?
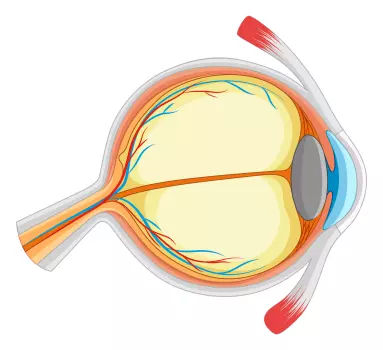
Glaucoma can occur without any cause, but many factors can affect it. The most important of these factors is intraocular eye pressure. Your eyes produce a fluid called aqueous humor that nourishes them. This liquid flows through your pupil to the front of your eye. In a healthy eye, the fluid leaves through the drainage canals located between your iris and cornea. With glaucoma, the resistance increases in your drainage canals which might be inherited from your parents. The fluid has nowhere to go, so it builds up in your eye. This excess fluid puts pressure on your eye. Eventually, this elevated eye pressure can damage your optic nerve and lead to glaucoma.
Signs & Symptoms

Severe headache

Severe eye pain

Nausea or vomiting

Blurred vision

Halos or colored rings around lights

Eye redness

difficulty seeing things in your central vision

Risk Factors

Age above 40 years

Family history of glaucoma

African, Hispanic, or Asian heritage

Elevated eye pressure

Farsighted or nearsighted vision

Prior eye injury

Prolonged use of steroid medications

Thin corneas at the centre

Optic nerve thinning

Concurrent health conditions like diabetes, migraines, high blood pressure, poor blood circulation, or systemic issues affect the whole body.
FAQ
1- What is glaucoma?
Glaucoma is a group of eye conditions that damage the optic nerve, which is responsible for transmitting visual signals from the eye to the brain. It is often caused by increased pressure in the eye and can lead to permanent vision loss if left untreated.
2- What are the risk factors for glaucoma?
The risk factors for glaucoma include age (being over 50 years old), family history of glaucoma, elevated intraocular pressure (IOP), near-sightedness, previous eye injuries or surgeries, and certain medical conditions such as diabetes, high blood pressure, and cardiovascular diseases.
3- What are the common symptoms of glaucoma?
In the early stages, glaucoma may not have any symptoms. One of the earliest indicators is frequent change of glasses. As the condition progresses, it may cause symptoms such as loss of peripheral field of vision, frontal headache, blurred vision, colored halos around lights and pain or redness in the eyes. Regular comprehensive eye examinations, including measurement of eye pressure, are essential for early detection of glaucoma especially in cases with a strong family history of glaucoma..
4- How is glaucoma diagnosed?
Glaucoma is diagnosed through a comprehensive eye examination that includes measuring intraocular pressure (IOP) by contact tonometry method, examining the optic nerve head and assessing the visual field. Additional tests, such as optical coherence tomography (OCT) and gonioscopy, may also be performed to determine the type and severity of glaucoma.
5- What are the treatment options for glaucoma?
The treatment options for glaucoma depend on the type and severity of the condition. The majority of patients are managed medically by lifelong eye drop therapy. The eye drops work in glaucoma by reducing the intraocular pressure. The other treatment options are oral medications, laser therapy, and surgery.
Expert Eye Specialist Glaucoma Treatment and Surgery in Mumbai
Can Glaucoma Be Stopped?
Glaucoma damage is permanent—it cannot be reversed. But medicine
and surgery help to stop further damage. To treat glaucoma, your
ophthalmologist may use one or more of the following treatments.
A) Medication
Glaucoma is usually controlled with eyedrop medicine. Used every day,
these eye drops lower eye pressure. Some do this by reducing the amount of
aqueous fluid the eye makes. Others reduce pressure by helping fluid flow
better through the drainage angle.
Never change or stop taking your glaucoma medications without talking to
your ophthalmologist.
B) Laser surgery
- Trabeculoplasty. This surgery is for people who have open-angle
glaucoma and can be used instead of or in addition to medications.
The eye surgeon uses a laser to make the drainage angle work
better. - Iridotomy. This is for people who have angle-closure glaucoma.
The ophthalmologist uses a laser to create a tiny hole in the iris.
This hole helps fluid flow to the drainage angle.
C) Surgery
- Trabeculectomy – This is where your eye surgeon creates a tiny flap
in the sclera. They will also create a bubble (like a pocket) in the
conjunctiva called a filtration bleb. It is usually hidden under the
upper eyelid and cannot be seen. Aqueous humor will be able to drain
out of the eye through the flap and into the bleb. In the bleb, the fluid
is absorbed by tissue around your eye, lowering eye pressure. - Glaucoma drainage devices – Your ophthalmologist may implant a
tiny drainage tube in your eye. The implant sends the fluid to a
collection area (called a reservoir). Your eye surgeon creates this
reservoir beneath the conjunctiva. The fluid is then absorbed into
nearby blood vessels. - Cataract surgery – For some people with narrow angles, removing
the eye’s natural lens can lower eye pressure. With narrow angles the
iris and the cornea are too close together. This can cover (block) the
eye’s drainage channel. Removing the eye’s lens with cataract surgery
creates more space for fluid to leave the eye. This can lower eye
pressure.
Your Role in Glaucoma Treatment – Only ‘YOU’ can save your vision !
Treating glaucoma successfully is a team effort between you and your
doctor. Your ophthalmologist will prescribe your glaucoma treatment. It is up to
you to follow your doctor’s instructions and use your eye drops.
Once you are taking medications for glaucoma, your ophthalmologist will
want to see you regularly. You can expect to visit your ophthalmologist about
every 3–6 months. However, this can vary depending on your treatment needs.
If you have any questions about your eyes or your treatment, talk to your
ophthalmologist.